One Door Closes…



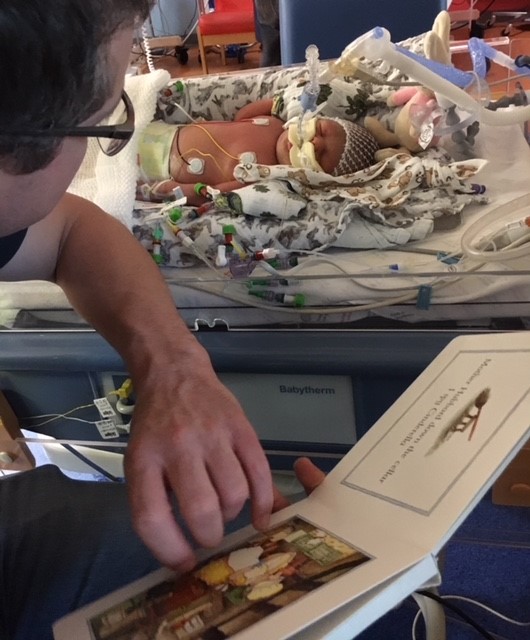
The breast feeding consultant will be referred to as Jackie, because I don’t remember her name or her actual job title, but I do remember that she was very knowledgeable in her field. She approached me and my mind flashed back to that first day momentarily. I had seen her before, she had brought the photo of Betty to my bedside and had me squeezing my boobs in no time. Jackie asked about my feeding preferences and I told her that I had originally hoped to breast feed exclusively, before this was taken from me. So I explained that I was no longer precious about breast feeding, that I would like to try but I was quite happy to accept that my baby may well be formula fed. And that is absolutely, perfectly and totally ok. In fact, I am pretty certain that as long as your baby is fed, and you don’t feed them broken glass, then its just fine. Anyway, I digress. My memory is hazy but I believe we continued to give Betty a combination of breast milk and formula via her NG tube. This day was different though. Betty was put to my boob and remarkably, she knew exactly what to do but had a little diffickty staying latched on. I blame my odd shape nipples for this and so I was offered a nipple shield. Whoever invented these things is in my opinion, a sadist! It was this flimsy piece of silicone that I was to place over by own nipple/boob, to give Betty something to latch onto. Well, the poor kid had never done any of this before and so my nipple or false nipple, she wasn’t getting it. Around the time I was attempting this nipple ridiculousness, I asked the nursing staff to remove Bettys NG tube for an hour. Her tube had become an object of play and she was constantly pulling at it which dislodged it, meaning it had to be fiddled with non-stop. The tube in place was looking grotty and I just didn’t like it so the nurse kindly removed it and agreed to re-tube when Betty’s next feed was due.
When said feed was due, the tube had to be replaced and Betty screamed bloody murder! She was clearly in discomfort and the nurse was unable to replace it. Jackie stepped up and managed, with quite a struggle, to re-insert the NG tube. A few hours laer Jackie appeared again, peeping her head around the wall I had created out of the screens on the ward. She asked me in a frank yet compassionate manner, how much I wanted to breast feed. I repeated what I had already tol her. That in an ideal world, yes I would have loved to, but now, I just wanted my baby fed so that I could take her home. And with that, Jackie asked if I would agree to the permanent removal of the NG tube. Im sure I said YES rather quickly and a little louder than she had expected! It was the last medical thing on my baby girl and I was desperate to see the back of that tube. I agreed to bottle feed Betty and continue to try putting her on my boob.
Enter Carol……! Mum had arrived for a visit during one of my attempts to breast feed my daughter. She asked if she could touch my boob…..ever the professional is my mum! Of course I handed her my consent and with that, she repositioned Betty, told me a few key pointers for breast feeding, and that was it. Betty was on the boob! She still had to have the formula and bottle to maintain her growth and to measure exactly what she was taking in. a benefit of bottle feeding I guess, is that you know exactly how much your bay has had. She would go on my boob intermittently and I often did this as ‘skin-to-skin’ as I wanted to make up for lost time.
I had overheard someone use the phrase ‘room-in’ and came to realise that this was a final step before taking your baby home. Someone mentioned it in passing to me and so when the Dr came round I mentioned it too. By the next ward round (two to three times a day in NICU) the assumption had been made that James and I were due to ‘room-in’ that very week. The beauty of gentle conversational manipulation (insert cheeky wink here!). Plans were made for me and James to sleep in the parent room (one of only two in the Portsmouth NICU) on the Thursday and Friday. We would be sleeping in this room with Betty! I hadn’t realised this when I started telling the staff that we were in fact, due to room-in that week….I was so excited, terrified, gleeful, panic stricken, but above all, I was starting to believe that I would take my baby home. That the thoughts I’d had during pregnancy of never bringing a baby home, were wrong. My baby girl was going to be having her first ever sleepover with her mum and dad. The two people that love her more than anything else in the whole universe. The two people who had waited and prayed and listened and watched and hoped for 5 weeks, they were getting their baby all to themselves. With no monitors!!!
The room that we all were due to stay in was actually decent for what it was. There was a shower which meant I could stay. I didn’t have to leave her for a whole 48 hours, how utterly blissful. In the lead up to this, James and I had written a list of things we had to do/Betty had to do in order to take her home. One Dr mentioned that a potential, discharge date for Betty would be June 30th 2018. That was Betty’s due date and so I jumped on it. It was a Saturday and so, in my experience, patients don’t tend to get discharged at the weekend but I clung on to it.
When the day came to room-in I had given James a list of things to bring in for me as I had packed in a fluster. When the evening turned to night and the night shift arrived, we were told we could take our baby to our room for the night. Any problems or concerns, the nurses were all on hand to step in. Once we were in the room it was surreal. Just the three of us, how I had imagined it being from the very start. Betty was settled and sleeping but I got her out of her hospital crib and put on my bed with me. I lay next to her, watching and listening to her breathing quietly, rhythmically. I don’t know what was going through my head at the time but I know that I was in awe of this little girl who had proved to be so strong in her short life so far. My little sausage is surely destined for great things.
The emphasis in our new found home-from-home, was very much on the parents taking the lead in the care of their baby. Medical interventions were to continue, Betty’s feeds were on a strict regime, much like a medication regime, and we adhered to this, naturally. I remember asking one of the night nurses how the oximeter would work in our private room away from the ward. She told me, quite frankly but with a hint of warmth, ‘you are the baby’s monitor’. And she was right, people that don’t go through the NICU journey would never dream of rigging their baby up to machines to check their heart rate and oxygen saturation level.
On our list we had made sure to detail the ‘car seat challenge’ which probably sounds much more fun than it actually is! The car seat challenge is a new protocol in place for NICU babies and their parents. I had witnessed this challenge being carried out when in Southampton when Mason’s mum had to put her baby in her car seat and then wait…..I hadn’t paid much attention to exactly what she was being asked to do. Mason was on oxygen and there was chatter about this, but I just looked over and felt a sense of genuine hope. They were on their way home and ticking off the final requirements before they did so. Mason’s mum, Amy, was a friendly face. One of those that you see and feel instantly settled in her company. She was a dab hand at NICU life and I got the impression she had been there a while. She had all her stuff, pillow, bits for her baby and a real sense of knowing what she was doing. This is most likely a persona she never thought she would have to portray, but she, like so many of us, had no other option. She had embraced her situation and did so with such grace and composure. My knowledge of the car seat challenge was minimal. I knew that Betty had to maintain stable observations for a period of time. I didn’t know that she had to maintain a stable heart rate and oxygen sats for a whole hour! Anyone that has put a baby into a car seat for the first time after 5 weeks of being flat in a cot, will know that they tend to be a bit miffed about the situation!
When we did our challenge, James had popped home so I had to deal with the slightly power crazy care assistant on my own. James had been put in charge of the car seat purchase as he is in the motor trade and that is his area of expertise. He had chosen the Joie swivel style of seat. It is (when we bought it) the safest on the market and can swivel around so you don’t need to struggle putting your baby in at that awkward angle. This means you can get them comfy and ensure the straps are all secure without having to do your back in at the same time. This type of car seat has an arm that goes from the care seat and onto the floor/foot well. It is fixed by the isofix dooda so it is considered much more secure than the old seat belt style, although I will stress here that I am not an expert in car seat safety. I’m just a really anxious mother!
I put Betty into the car seat and she was not happy. She settled for short periods but she was mostly really quite pissed off. What made this more difficult was that the staff had not completed the car seat challenge with a car seat like ours. So they had no way of replicating the actual angle of the car. With a traditional car seat, you can place it on the floor and it sits nicely, baby can go in like this and then be transferred to the car. With our model, when placed on the floor, the arm that is designed to sit on the floor of the car, makes the whole seat look really wonky. The care assistant had tried to prop the arm up to complete the test but it was a shoddy piece of DIY and to no surprise, Betty failed the car seat challenge quite miserably!
I told the care assistant that I would walk her home in her pram if I had to! What do people do that don’t drive?! The bloody bus seat challenge?! No, of course they don’t (eye roll!). I do understand the importance of this test, please don’t mistake my sarcasm and cynicism for ignorance. I know that it is vitally important to ensure the parents are aware what level of oxygen their bay needs when in the car seat. The level of oxygen required will differ to their normal requirement due to the position of the car seat. We all breathe differently in different positions but for most of us, we don’t even notice. But a baby on oxygen will struggle to saturate appropriately in different positions. But my baby, unlike Amy’s, was not on oxygen. She had failed this new test because she simply did not like being in the car seat, or so it originally seemed. I spoke to James who was instantly irritated but calm and asked about the position of the seat etc etc. I agreed with the care assistant that we would try again later in the day. I asked to do the test away from the many toddlers running around being loud, which didn’t help the first attempt. At around 2pm we restarted the test, this time without the new-born insert that was recommended for the car seat and babies of a normal new-born weight, which Betty still was not. Nevertheless I lovingly placed my little girl into the newly positioned car seat. And I sat next to her, staring at the monitors and praying for stable readings. My prayers were answered and she passed. Even with the new power crazed care assistant insisting that the test had started at 2:15 so made Betty stay in the seat an extra 15 minutes. Unnecessary but I, for once in my life, was not going to argue. I had Saturday June 30th etched in my brain. I was taking my baby home!
When James arrived back at the unit we had a debrief of the day’s events. He commented that I seemed angry, something I hadn’t been in 5 weeks. And he reminded me that now, in that moment, I was able to be angry with the situation. Before that time, anger was not an emotion I had even mustered. Now the crisis had passed. Now that we were simply jumping through hoops, I was getting short tempered with the hoops. And rightly so I think, they were stupid poxy hoops.
The next day a friendly consultant came to see Betty. He was to carry out a final brain scan, Betty’s fourth in 5 weeks. He spoke to me as he did it. He told me that the bleed on Betty’s brain had cleared and it all looked completely normal. I didn’t know she’d had a bleed on the brain until he said it. I’m glad I didn’t know, I didn’t need that on my mind as well as everything else.
James and I, with the help of the staff at QA NICU, had worked our way through the list of jobs to do. It was Friday 29th June 2018. We were waiting for ward round in the afternoon. A female consultant this time. She confirmed discharge for the following day.
At some point in this week back at QA, I had called Kim and asked if she wanted to come and see Betty. She said yes, of course she did! I also had my auntie Nicky and her partner Chris come to see us. Nicky is a mum of two wonderful boys. Her boys are men now and they are a credit to her and my uncle. Nicky is one of the most honest people I know. She cares deeply for the people in her life and I am lucky to be one of those people. I remember her coming into the room, being told rather abruptly, to wash her hands and we grinned at each other. I don’t remember what we talked about but I remember how she looked at me and Betty. That feeling of knowing my baby was so loved by the people I love the most was and is the most humbling feeling in the world.
Friday night is a blur. I know that my mind set of ‘hope for the best, expect the worst’ was more relevant now than I thought possible. Thoughts of, what if she dies in her sleep the night before we are due to take her home? What if the Dr on shift the next day finds something wrong with her and stops her discharge? The list of intrusive thoughts is limitless. But, Saturday came. We got Betty ready and James took her to the ward. I showered and made myself as presentable as I could. We waited for the paperwork and Dr T was there! The man that saved Bettys life was there. He offered us yellow card access to child assessment. Yellow card in Portsmouth is direct access to children’s assessment. It means you bypass GP, 111, A&E. You call them and go straight in. This was reassuring. To know if we had any concerns at all, we could go straight into an assessment area and be seen, that was and still is, priceless. When people say we are lucky to have this, I just smile. I don’t need to tell them all of this. They can read this blog if they wish. But I don’t need to justify why my child has priority. I know why. And I know that it is warranted.
James went to the car to get the pram. The pram I had last seen in John Lewis when Sue had kindly bought it for us. He wheeled it in and my heart flipped. I picked Betty up. I held her, smelled her neck, kissed her and gently placed her in her carriage. We had all the paperwork we needed. James had already loaded the car with our stuff and so we were good to go. Someone took photos of us, maybe a nurse but I’m not sure.
We put her in the car seat, still without the new born insert, and off we went. I had asked James to make sure no one came out to see us. We live on a main road and our house is attached to the showroom that James and his family own so his dad and possibly his mum would be there. I just wanted to take her through the front door on our own, without anyone else to consider. As always, James family were respectful of my wishes and in we all went. James’s dad had had a gorgeous hand drawn sign made which simply said ‘welcome home Betty’ with a picture of a pram on it. We stood inside our front door, in front of the mirror I used to routinely check myself in before I left the house, and we cried. We cried tears of joy, relief, giddy happiness, relief, everything. Everything from the past 5 weeks we stood and shed. We slowly moved through to the lounge where we stayed for the rest of the day. The heat was new to me. I had only experienced brief periods of the heatwave, so sitting in a lounge that was 24 degrees was new. It was refreshing compared to the air conditioned hospitals we’d treated as home for past few weeks. Betty slept. Betty slept on me, on James, in her new Moses basket. She was home. I am sure she knew that. Everyone knows when they’re home.
This wasn’t the end of our journey. We are still very much on it. This marked the end of living in hospital, being told when we could touch or hold our baby. It was the closure of one door and the opening of another.
This blog reflects on my experience and if you speak to James, you will get a very different perspective on what happened. James will talk of facts, figures, actual words spoken. I remember the bad bits mostly and I am thankful for James. He became my everything. Before we had Betty I was guarded with James to some degree. But going through hell and having him by my side has shown me who he is, who I am and who we are when we are together. I do not gush about how I feel about James, not to him or anyone. I’m not that way, hearts and flowers make me shudder to be honest. But what I have in James is a soul mate. The person I want to see. The person I want to tell everything. The person who has seen me at my lowest, my most vulnerable, at my very breaking point. He is more than hearts and flowers. He is the love of my life. He showed me and Betty the purest devotion, love and compassion while all the time, going through the very same trauma. James coped far better than I did. James continues to cope far better than me! But knowing he will always be objective, honest, kind and will go to the end of the earth for me and Betty, makes me want to wake up next to him every day.
For me, the time I spent in NICU changed me. I am still me, I am still abrasive, honest (maybe too honest at times), angry, hyperactive and hostile when I want to be. But, I see everything differently now. I don’t judge others so quickly and I always look at what people are doing and think about why. I wonder what people are suffering that they don’t share with the world. I chose to document our/my journey because I find it helpful. Some people choose to keep their experiences private and that is also fine. Everyone copes differently with the events that this universe sends us and it is not my place, or anyone else’s, to judge how people deal with theirs.
I have and am still, re-evaluating my own life, career, desires. I no longer see work as a must. It is something I will choose to do. And in time, I will do something that brings me much more joy. My whole life is now focused on my little girl, the little life that fought so hard to be here with me. Everything I do is for her. I surround myself with people that bring me joy, pleasure, happiness and laughs. I have and will continue to distance myself from negative energy, in whatever form it comes. I have offended people with this blog and it saddens me that some people, especially members of my own family, can treat me with such disdain when I have done nothing wrong. I have spoken of my experience and my experience only. For those that choose to make my story about them, they are no longer a part of my life. This happened far closer to home than I could ever have imagined and my career is likely a curse at times as it leads me to see people in a light that others are unable to see. I have distanced myself from this situation and from all situations that make me doubt myself. I am me. I am a good mum, I am a fun mum, and I am definitely on my way to being a very embarrassing mum! My baby is happy. Betty laughs from morning til night and is a content and beautiful soul. And, I am happy.
I will be in debt to the medical and nursing teams that worked tirelessly to bring our daughter to full health, and in particular to Dr T. Without his determination in the first 27 minutes of Betty’s life, we would not have our darling girl as we do now. We remain under the care of Dr T as outpatients and until recently were also under the genetics team. We still have no answers. There is still no known cause for Betty’s hydrops and it is very likely that we will never know why or how this happened. In future pregnancies I will be under Mr SG, the obstetrician who identified Betty’s hydrops in utero and I trust him. We want to have more children and I understand that the pregnancy will be very difficult for me, if not physically then certainly mentally. But we would like Betty to have a sibling. And so I will have to accept what the universe sends our way. I will of course, hope for the best but expect the worst. There is no reason that a future pregnancy should have the same complications as before but because it has happened before, the risk is there.
If you have never been through NICU, if you have had your children and been sent home with a healthy baby within a few days, please count your blessings. Please appreciate what you have. I see and hear of people behaving in ways which make me believe they have no idea how lucky they are. To never experience being told that your baby may very well die, and having to stand by and watch, helplessly, it changes a person. If you have never had to worry that your baby may not develop normally because they had a bleed on the brain, count your blessings. I know that you can never truly know what I went through, but I am hoping this might help. Being a NICU mum or dad, changes you forever and you become a far more refined version of the original you. NICU parents love in a slightly unique way, not to say we love our children more than other people do, but it is a unique and very special love that we have for our little ones. It is being part of a group of people you never thought you would be. NICU parents, I salute you all. To everyone I met, I think you’re all incredible, strong, kind and just amazing people!
Always hold your little ones close for a bit longer. Always tell them you love them. Always hold their hand, sniff their neck as you hug them, look at every detail of their toes. I still do this everyday. Because every single day I am thankful for the beautiful gift I have been given. And, she has really cute toes so…..
Please continue to share this blog. The most important thing is that no one else has to go through what we did. And if someone is going through a similar journey, I hope that this blog may offer some comfort.
Thank you for reading. I will post more about coming home so stay tuned……. Much love xxx










Recent Comments